1. Arterial hypertension
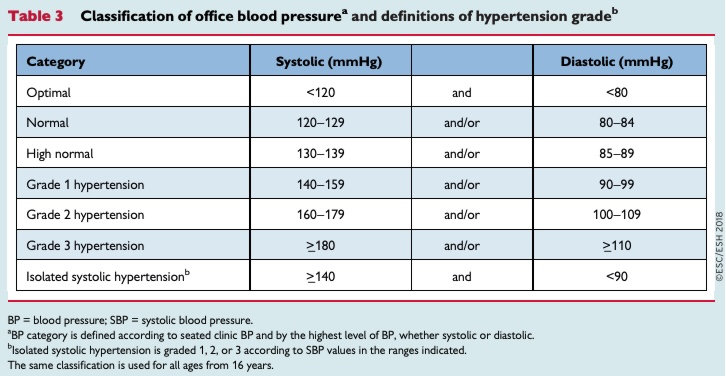
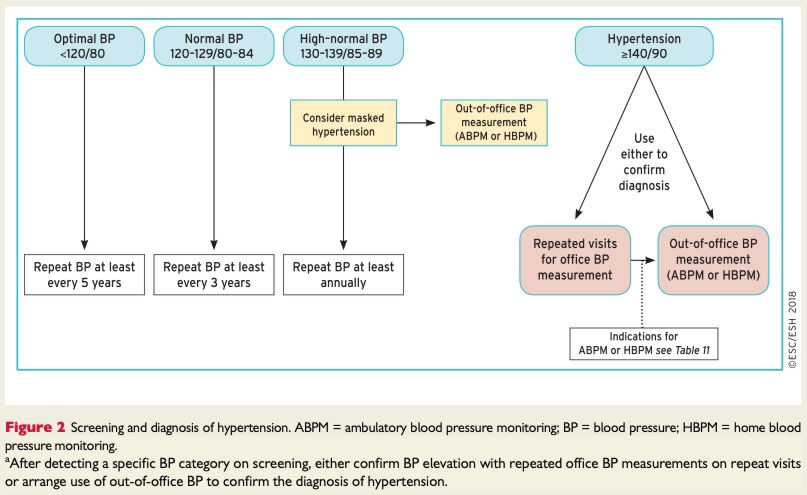
Hypertension is defined as office SBP values >= 140 mmHg and/or diastolic BP (DBP) values >= 90 mmHg
White-coat hypertension refers to the untreated condition in which BP is elevated in the office, but is normal when measured by ABPMAmbulatory Blood Pressure Monitoring, HBPMHome Blood Pressure Monitoring, or both. Conversely, masked hypertension refers to untreated patients in whom the BP is normal in the office, but is elevated when measured by HBPM or ABPM.
Hypertension is defined as resistant to treatment when the recommended treatment strategy fails to lower office SBP and DBP values to <140 mmHg and/or <90 mmHg, respectively, and the inadequate control of BP is confirmed by ABPM or HBPM in patients whose adherence to therapy has been confirmed. The recommended treatment strategy should include appropriate lifestyle measures and treatment with optimal or best-tolerated doses of three or more drugs, which should include a diuretic, typically an ACEAngiotensin Converting Enzyme inhibitor or an ARBAngiotensin II Receptor Blocker, and a CCBCa Channel Blocker.
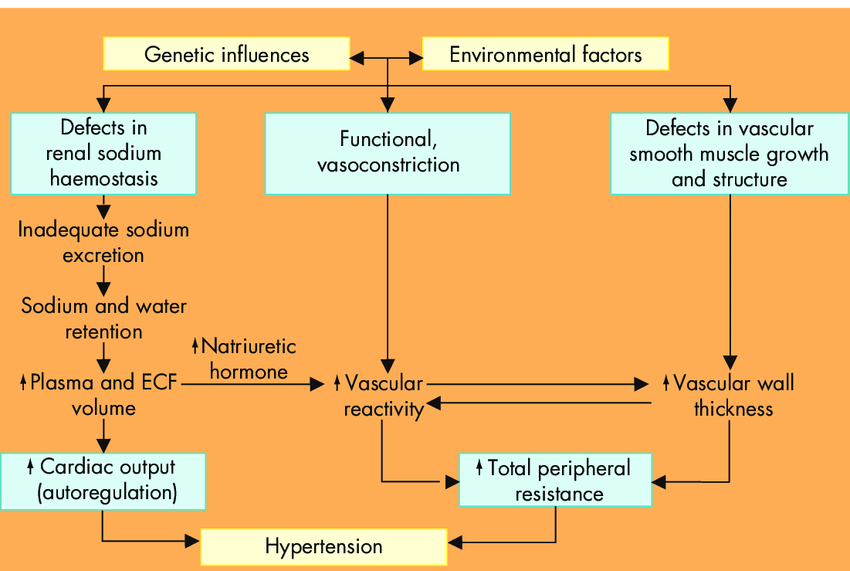
Pathogenesis
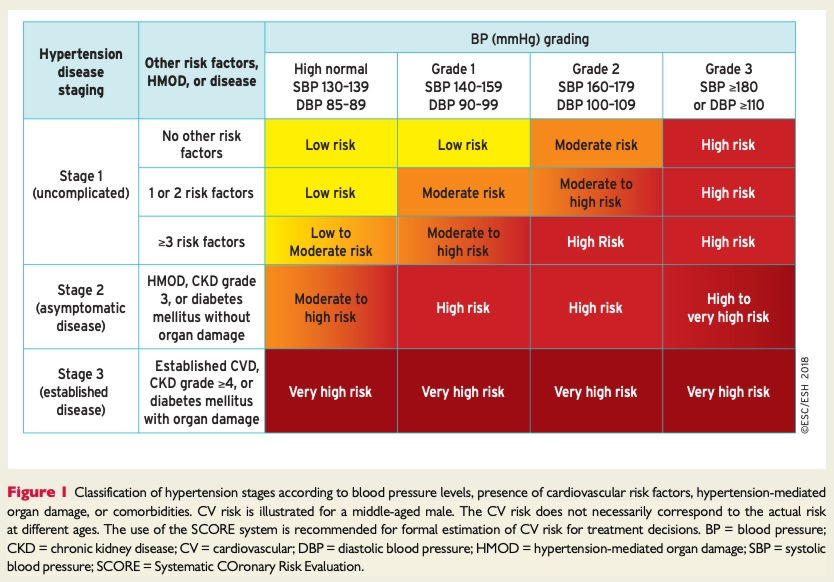
Classification
Etiology
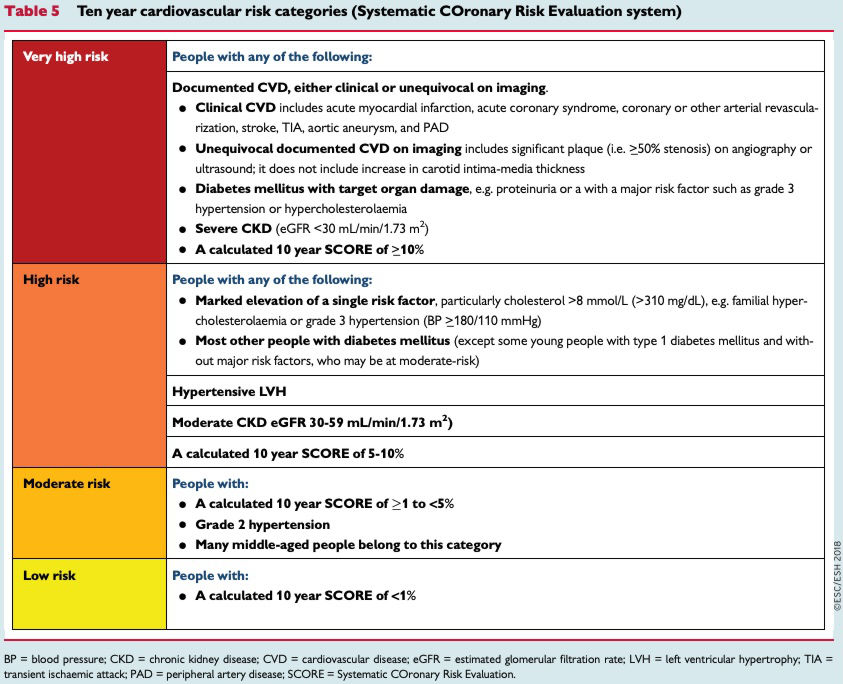
Cardiovascular risk factors estimated by the Systemic COronary Risk Evaluation (SCORE) system:
- Social deprivation, the origin of many causes of CVD
- Obesity (measured by BMI) and central obesity (measured by waist circumference)
- Physical inactivity
- Psychosocial stress, including vital exhaustion
- Family history of premature CVD (occurring at age <55 years in men and <60 years in women)
- Autoimmune and other inflammatory disorders
- Major psychiatric disorders
- Treatment for infection with human immunodeficiency virus
- Atrial fibrillation
- LV hypertrophy
- CKD
- Obstructive sleep apnoea syndrome
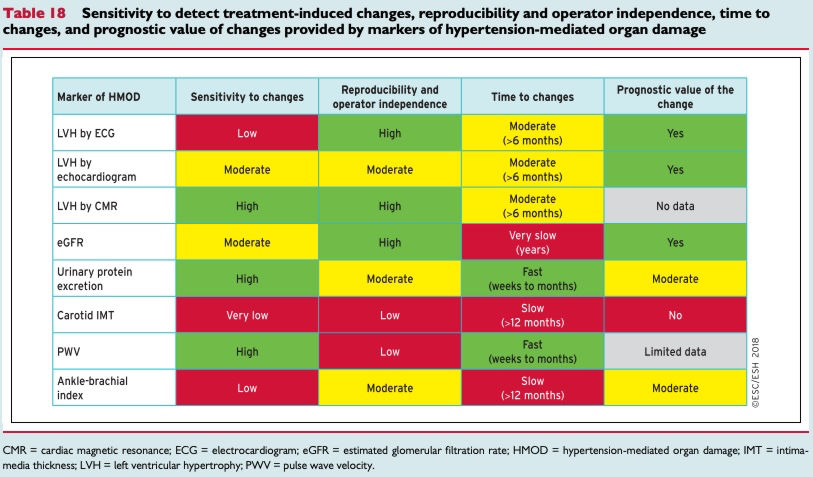
Diagnostics
Clinical
- Brain and eyes: headache, vertigo, syncope, impaired vision, TIA, sensory or motor deficit, stroke, carotid revascularization, cognitive impairment, dementia (in the elderly)
- Heart: chest pain, shortness of breath, oedema, myocardial infarction, coronary revascularization, syncope, history of palpitations, arrhythmias (especially AF), heart failure
- Kidney: thirst, polyuria, nocturia, haematuria, urinary tract infections
- Peripheral arteries: cold extremities, intermittent claudication, painfree walking distance, pain at rest, peripheral revascularization
Physical examination
Body habitus
- Weight and height measured on a calibrated scale, with calculation of BMI
- Waist circumference
Signs of HMOD
- Neurological examination and cognitive status
- Fundoscopic examination for hypertensive retinopathy
- Palpation and auscultation of heart and carotid arteries
- Palpation of peripheral arteries
- Comparison of BP in both arms (at least once)
Secondary hypertension
- Skin inspection: cafe-au-lait patches of neurofibromatosis
- (phaeochromocytoma)
- Kidney palpation for signs of renal enlargement in polycystic kidney disease
- Auscultation of heart and renal arteries for murmurs or bruits
- indicative of aortic coarctation, or renovascular hypertension
- Comparison of radial with femoral pulse: to detect radio-femoral delay in aortic coarctation
- Signs of Cushing’s disease or acromegaly
- Signs of thyroid disease
Lab tests
- Haemoglobin and/or haematocrit
- Fasting blood glucose and glycated HbA1c
- Blood lipids: total cholesterol, LDL cholesterol, HDL
- cholesterol
- Blood triglycerides
- Blood potassium and sodium
- Blood uric acid
- Blood creatinine and eGFR
- Blood liver function tests
- Urine analysis: microscopic examination; urinary protein by dipstick test or, ideally, albumin:creatinine ratio
- 12-lead ECG
Diagnosis
DDx
Suspect secondary hypertension:
- Younger patients (<40 years) with grade 2 hypertension or onset of any grade of hypertension in childhood
- Acute worsening hypertension in patients with previously documented chronically stable normotension
- Resistant hypertension
- Severe (grade 3) hypertension or a hypertension emergency
- Presence of extensive HMOD
- Clinical or biochemical features suggestive of endocrine causes of hypertension or CKD
- Clinical features suggestive of obstructive sleep apnoea
- Symptoms suggestive of phaeochromocytoma or family history of phaeochromocytoma
Treatment
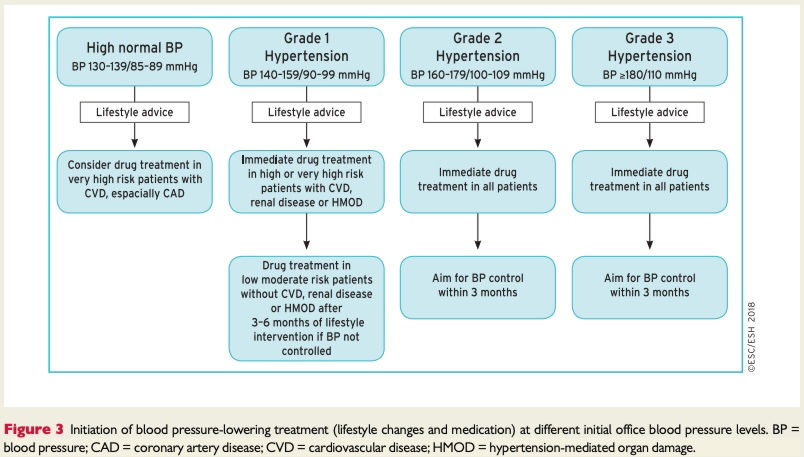
First objective of treatment: lower BP to <140/90 mmHg, and if the treatment is well tolerated, target 130/80 mmHg or lower in most patients
Lifestyle interventions
- salt restriction (< 5 g/day),
- moderation of alcohol consumption,
- high consumption of vegetables and fruits,
- weight reduction and maintaining an ideal body weight,
- regular physical activity
- smoking cessation and other lifestyle measures are also important beyond BP (i.e. for CVD and cancer prevention)
Medication
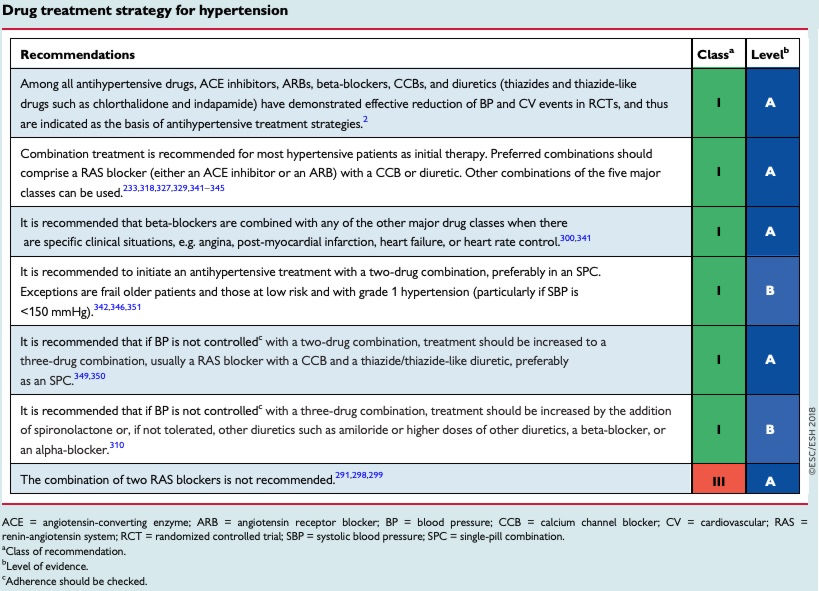
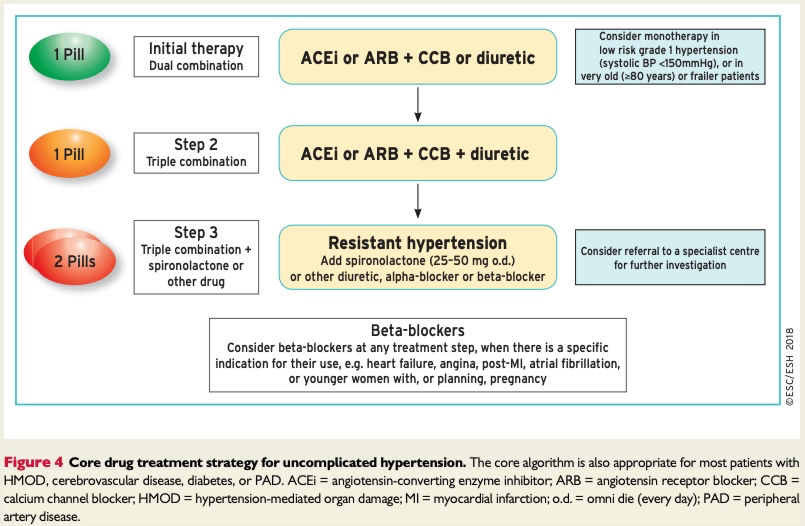
- The initiation of treatment in most patients with an SPC comprising two drugs, to improve the speed, efficiency, and predictability of BP control.
- Preferred two-drug combinations are a RAS blocker with a CCB or a diuretic. A beta-blocker in combination with a diuretic or any drug from the other major classes is an alternative when there is a specific indication for a beta-blocker, e.g. angina, post-myocardial infarction, heart failure, or heart rate control.
- Use monotherapy for low-risk patients with stage 1 hypertension whose SBP is <150 mmHg, very high-risk patients with high–normal BP, or frail older patients.
- The use of a three-drug SPC comprising a RAS blocker, a CCB, and a diuretic if BP is not controlled by a two-drug SPC.
- The addition of spironolactone for the treatment of resistant hypertension, unless contraindicated (see section 8.1.4).
- The use of other classes of antihypertensive drugs in the rare circumstances in which BP is not controlled by the above treatments.
- Information on availability and recommended doses of individual drugs, as well as SPCs and free combinations, can be found in national formularies.
(see the guidelines1 for treatment strategies in other complications and the management in pregnancy)
First aid
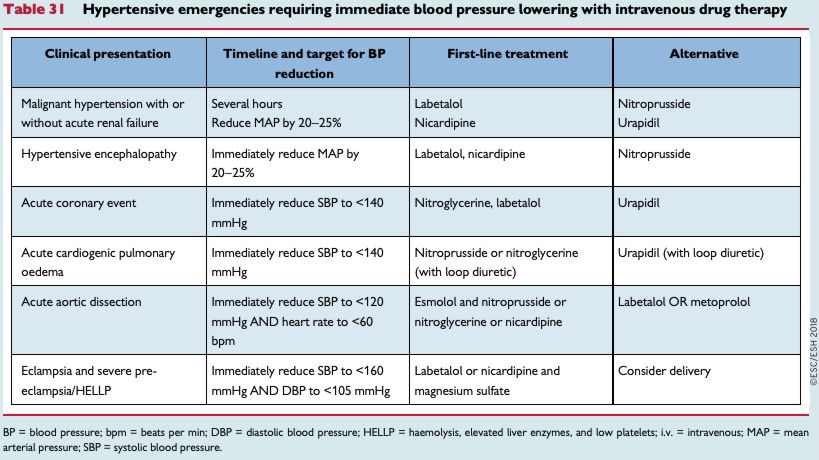
Typical presentations of a hypertension emergency are:
- Patients with malignant hypertension characterized by severe hypertension (usually grade 3) associated with funduscopic changes (flame haemorrhages and/or papilloedema), microangiopathy, and disseminated intravascular coagulation, and can be associated with encephalopathy (in about 15% of cases). The term ‘malignant’ reflects the very poor prognosis for this condition if untreated.
- Patients with severe hypertension associated with other clinical conditions
- Patients with sudden severe hypertension due to phaeochromocytoma
- Pregnant women with severe hypertension or preeclampsia
Complications
- Heart. Chronically increased left ventricular (LV) workload in hypertensive patients can result in LVH, impaired LV relaxation, left atrial enlargement, an increased risk of arrhythmias, especially AF, and an increased risk of heart failure with preserved ejection fraction (HFpEF) and heart failure with reduced ejection fraction (HFrEF).
- Vascular. Atherosclerosis, plaques, large artery stiffness
- Kidney. Chronic Kidney Disease
- Hypertensive retionpathy
- Brain. Transient ischaemic attack (TIA) and stroke